Diabetes, a chronic medical condition marked by high blood sugar levels, affects millions of people worldwide. This disease has widespread implications throughout the body, with the feet often being a particular area of concern. High blood sugar levels can lead to a multitude of foot-related complications, collectively known as diabetic foot problems. These problems, if left untreated, can result in serious health issues such as infection, ulceration, and even amputation. Understanding the symptoms and taking proactive steps towards treatment and prevention can significantly improve the quality of life for those living with diabetes.
About Diabetic Foot Problems
Diabetic foot problems arise primarily due to two key complications related to diabetes: peripheral neuropathy and peripheral artery disease. Peripheral neuropathy is a condition marked by damage to the peripheral nerves, often causing weakness, numbness, and pain in the feet and hands. This loss of sensation makes it difficult for patients to feel foot injuries, which could lead to unnoticed and untreated wounds.
Peripheral artery disease, on the other hand, reduces blood flow to the feet, making it hard for sores or infections to heal. Furthermore, diabetes can alter the biomechanics of the foot, leading to abnormal pressure points that can cause calluses and ulcers.
The combination of these factors puts those with diabetes at a high risk for foot complications, which can escalate quickly if not carefully monitored.
Common Symptoms of Diabetic Feet
Recognizing the symptoms of diabetic foot problems is the first step towards proactive management. Common symptoms may include:
- Numbness or tingling in the feet
- Pain or discomfort in the legs or feet
- Dry, cracked skin, especially on the soles
- Slow healing sores or cuts
- Ingrown or fungal toenails
- Corns and calluses
- Foot deformities such as hammertoes or bunions
- Cold or insensate feet
Changes in color, temperature, or swelling may also indicate a problem. Any of these symptoms should prompt immediate medical attention to prevent further complications.
How To Treat Diabetic Foot Problems
The treatment of diabetic foot problems is multifaceted and should ideally involve a team of healthcare professionals, including a podiatrist. Here are some key treatment strategies:
- Glycemic Control: The first step in treating any diabetic complication is managing blood sugar levels. Good glycemic control can slow the progression of neuropathy and improve blood flow to the feet.
- Foot Care: Daily foot inspection for signs of injury, infection, or change is crucial. Gentle washing and thorough drying, especially between the toes, can prevent fungal infections.
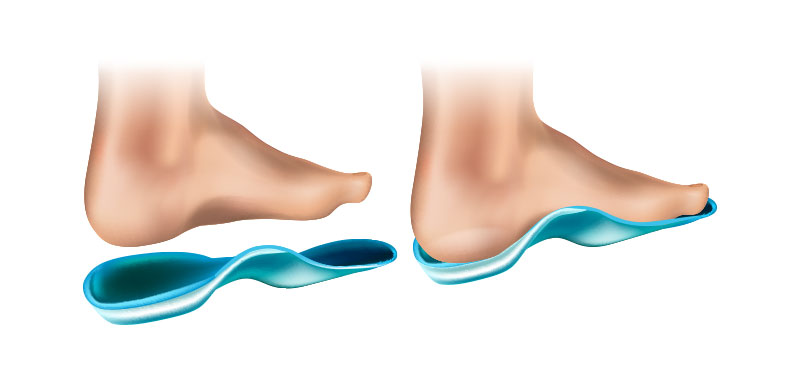
- Footwear: Patients should wear well-fitted shoes to prevent pressure points and blisters. Avoid going barefoot, even at home, to reduce the risk of injury.
- Wound Care: Wounds should be cleaned and dressed promptly. Non-healing wounds, signs of infection (like redness, warmth, or pus), or deep wounds should be evaluated by a healthcare provider.
- Professional Foot Care: Regular visits to a podiatrist can help identify and manage foot problems early. A podiatrist can help with toenail care, callus removal, and choosing appropriate footwear.
Diabetic Foot FAQs
Can diabetic foot problems be reversed?
A: While some nerve damage is irreversible, strict glycemic control and foot care can halt the progression and even improve some symptoms.
How often should a person with diabetes inspect their feet?
A: Feet should be inspected daily. Any changes or injuries should prompt a visit to a healthcare provider.
Can people with diabetes use over-the-counter treatments for corns or calluses?
A: People with diabetes should not use over-the-counter treatments for corns or calluses without consulting their healthcare provider. These treatments can cause skin damage and ulcers.
What type of footwear is recommended for a person with diabetes?
A: Comfortable, well-fitted shoes that do not rub or cause pressure points are recommended. Shoes should have a roomy toe box, and materials like leather that allow the foot to breathe are preferable.
Is it normal for people with diabetes to have cold feet?
A: Cold feet can be a sign of poor circulation, which is common in diabetes. However, it’s always important to discuss new or changing symptoms with your healthcare provider.
Why are people with diabetes more prone to foot problems?
A: High blood glucose levels can lead to damage to various tissues in the body, including nerves and blood vessels. In the feet, this can result in peripheral neuropathy (loss of sensation) and peripheral artery disease (reduced blood supply). When the sensation is decreased, a person might not feel a minor cut or scrape, which can then go unnoticed and develop into a more serious wound or infection. Poor circulation can further delay wound healing, increasing the risk of infection and ulcers.
What are the signs of foot problems related to diabetes?
A: Signs of foot problems in diabetes can include a loss of sensation, changes in the shape of your feet, dry and cracked skin, especially around the heel, sores or ulcers that do not heal, tingling or burning sensation, sharp pains, changes in skin color, temperature changes (especially increased warmth), and ingrown or fungal toenails. If you notice any of these signs, it is important to see a healthcare provider promptly.
How can I prevent foot problems if I have diabetes?
A: Prevention includes good diabetic control to minimize the risk of neuropathy and blood vessel disease. Daily inspection of the feet to catch any minor injuries or changes early, good foot hygiene, wearing well-fitting shoes, and regular podiatry visits for foot care are also very important. Regular exercise can improve circulation, and quitting smoking is important to improve blood vessel health.
What are the long-term complications of untreated or poorly managed diabetic foot conditions?
A: Long-term complications of untreated or poorly managed diabetic foot conditions can be severe. They can include chronic pain, persistent infection, development of gangrene (tissue death), and potentially amputation of the foot or lower limb. Additionally, chronic foot ulcers and ongoing infections can lead to a decreased quality of life and mobility, and increased dependence on others for day-to-day activities.
Diabetic foot problems can significantly impact a person’s health and quality of life. However, through understanding, vigilance, and proper care, these issues can be managed effectively, preventing further complications. As with any health issue, communication with healthcare providers is key.